In early 2003, the Institute of Medicine (IOM) released its report, Priority Areas for National Action: Transforming Health Care Quality. The report listed 20 clinical topics for which "best practices" were strongly supported by clinical evidence. The report documents the disappointingly low rates at which these practices have been implemented in the U.S., at an annual cost of many thousands of lives. To bring data to bear on the quality improvement opportunities articulated in the IOM's 2003 report, the Agency for Healthcare Research and Quality (AHRQ) engaged the Stanford-UCSF Evidence-based Practice Center (EPC) to perform a critical analysis of the existing literature on quality improvement strategies for a selection of the 20 disease and practice priorities noted in the IOM Report. Rather than concentrating on the specific clinical practices that appear to improve health outcomes, the focus of this review is on translating research into practice-identifying those activities that increase the rate at which practices regarded as effective are applied to patient care in real world settings. This report focuses on the clinical problem of hypertension. It, like the other reports in the series, aims to help readers assess whether the evidence suggests that a quality improvement strategy would work in their specific practice or with their specific patient population. The question of whether these may be crosscutting practices-that is, the manner in which those that have been studied for specific conditions such as hypertension might be applicable to others, such as asthma-remains to be seen. We defined the quality gap as the difference between health care processes or outcomes observed in practice, and those potentially obtainable on the basis of current professional knowledge. We defined a quality improvement (QI) strategy as an intervention aimed at reducing the quality gap for a group of patients representative of those encountered in routine practice. Finally, a quality improvement target is an outcome, process, or structure that the QI strategy aims to influence, with the goal of reducing the quality gap. Examples of targets relevant to this volume include outcomes such as reductions in blood pressure, or processes such as improved provider adherence with medication choices in patients with hypertension. Despite the importance and prevalence of both diabetes and hypertension, and the richness of their clinical literatures, studies that would help patients, providers, and policymakers choose how best to close their quality gaps are somewhat confusing. For each entity, certain strategies (such as the use of multifaceted interventions, and perhaps disease management in diabetes, and the adoption of organizational change in hypertension) appear to be more effective than others. Yet, even in these areas, problems with publication bias, co-interventions, and secular trends make sweeping conclusions hazardous. Our review provides a huge collection of research data for the interested reader to dissect; undoubtedly, there is information that will be directly applicable to a given clinical situation or location. There are several important questions that warrant consideration in the realm of hypertension quality improvement. Some of these questions focus on prevention (screening) while others relate to the management of a chronic disease (blood pressure control). The reviewers have selected the following questions as important foci in the development of this report: Which QI strategies improve the process of screening for hypertension? Which QI strategies most effectively ensure that blood pressure goals are achieved and maintained? Which QI strategies improve provider adherence to recommended guidelines for hypertension management? Which QI strategies improve patient adherence to hypertension treatment?
| FindBook |
有 1 項符合
Closing the Quality Gap: a Critical Analysis of Quality Improvement Strategies: Hypertension Care的圖書 |
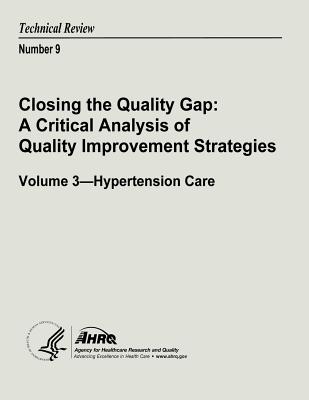 |
Closing the Quality Gap: a Critical Analysis of Quality Improvement Strategies: Hypertension Care 作者:U. S. Department of Health and Human Services(COR)/ Agency for Healthcare Research and Quality (COR) 出版社:Createspace Independent Publishing Platform 出版日期:2013-06-07 語言:英文 規格:平裝 / 110頁 / 27.9 x 21.6 x 0.5 cm / 普通級 |
| 圖書館借閱 |
| 國家圖書館 | 全國圖書書目資訊網 | 國立公共資訊圖書館 | 電子書服務平台 | MetaCat 跨館整合查詢 |
| 臺北市立圖書館 | 新北市立圖書館 | 基隆市公共圖書館 | 桃園市立圖書館 | 新竹縣公共圖書館 |
| 苗栗縣立圖書館 | 臺中市立圖書館 | 彰化縣公共圖書館 | 南投縣文化局 | 雲林縣公共圖書館 |
| 嘉義縣圖書館 | 臺南市立圖書館 | 高雄市立圖書館 | 屏東縣公共圖書館 | 宜蘭縣公共圖書館 |
| 花蓮縣文化局 | 臺東縣文化處 |
|
|
圖書介紹 - 資料來源:博客來 評分:
圖書名稱:Closing the Quality Gap: a Critical Analysis of Quality Improvement Strategies: Hypertension Care
|